Can you tell us a little bit about yourself?
I’m 48 years old. I’m an artist. I never went to school for it, my highest level of education is a GED, but I’ve been doing graffiti art for a long time, and I loved it since I was a kid in New York and Puerto Rico.
So you spent your childhood between those two places?
Yeah, I was born here, then moved to Puerto Rico and back a few times, coming back for good when I was 13, after my mother left my father. That last move was really bad for me, because I felt so alone here, and didn’t have friends in school. I missed the countryside of Puerto Rico.
When did your drug use start? And what were your drugs of choice?
When we moved back to New York the second time, when I was 13. I had no friends over here besides my cousins. One week in New York and I’m already smoking weed with my cousins, who were just a few years older than me.
I tried heroin at 15 with an older cousin, and didn’t try it again until 22 or 23. I was snorting it.
What was your drug use like in your 20s?
When I was younger, I was pretty successful, things were going well, I was kind of a playboy.
Heroin enhanced sex for me, so I liked that. I didn’t do it every day, because I knew I’d get addicted to it. I’d use on a Saturday and then not pick it up for weeks. After a couple years, I started liking it more and more, and then I was totally addicted. And cocaine was more or less the same thing.
So sex was a trigger for heroin?
Back then, yes. Now, it’s more just that if I don’t use, I feel in pain.
Cocaine was more to function, because at times when I was trying to work to earn as much money as possible, I was always tired so I had to take cocaine to stay awake.
What do you do for work?
I’m an artist. I get paid for making the graffiti murals on campuses. Apparel, painting, and all sorts of other work. You can follow me on Instagram @kerznyc.
It sounds like you’ve always been conscious of not building a dependence. Have you tried Medication-assisted treatment before?
I started taking Methadone in 2013, but I’m trying to cut down to a small dose and eventually transition to Suboxone. I’ve reduced my heroin use, but I’m still using, so I want to get off heroin. Especially now, with all the new chemicals in the drug supply, I can feel the xylazine and fentanyl in the batches I take.
Have you overdosed before?
I’ve overdosed at least 12 times, all before I started Methadone in 2013, and back then it was just heroin, none of the stuff in the supply now. Sometimes it was friends, sometimes paramedics who revived me. One time I was in a park and I was super out of it, and the only reason I lived is because a lady walking her dog saw me, and called the ambulance. If she hadn’t seen me, I would’ve died. God had that lady walking through there at night for a reason.
Every year, I go back to the park where this happened, in the Bronx, and I touch the tree where I was when the lady saved me. I call it the tree of life.
That’s beautiful. So if you’re still actively taking heroin, and sometimes cocaine, but haven’t overdosed in 11 years, is that just good luck, or what?
Now I ALWAYS test my drugs. If I don’t know my supplier, I’ll just take a half a bag at first, to make sure it’s cool. And being able to test my drugs with the test strips you’ve got here at Alliance, that’s big.
How long have you been coming to Alliance for Positive Change?
I found Alliance about 5 years ago, when you were on Allen St. I came here for the syringe exchange, because I never wanted to share needles, and I appreciated that the people running the syringe exchange never judged me. Actually, they congratulated me for being safer about my use, getting sterile syringes. I used to come here just for needles, now that’s the thing I need the least here. I probably come here for needles once every 40 times. I come here for coffee, for a safe place to hang out, especially when it’s super hot or super cold, because I’ve experienced homelessness for a long time, and I can’t stay on friends’ couches all the time.
A lot of the people we serve are experiencing homelessness. That’s a tough situation when you’re trying to change behaviors.
Oh yeah, the shelter system is really tough. You’ve got to find a good place where they actually treat you like a person, not like your parole officer. I’ve stayed at places like that, where every few weeks they’ll move you around—if you don't do this you lose your bed, it’s really messed up.
Now I’ve got a room in a shelter that doesn’t make you check in all the time, it’s pretty cool, and I applied for Section 8 housing. Some of the case managers here are helping me take the housing vouchers to try to find an apartment. I want a safe place to live, so I can take care of my physical health.
How has your drug use changed since you’ve been coming here?
My drug use is way down, and when I use, I use way less.
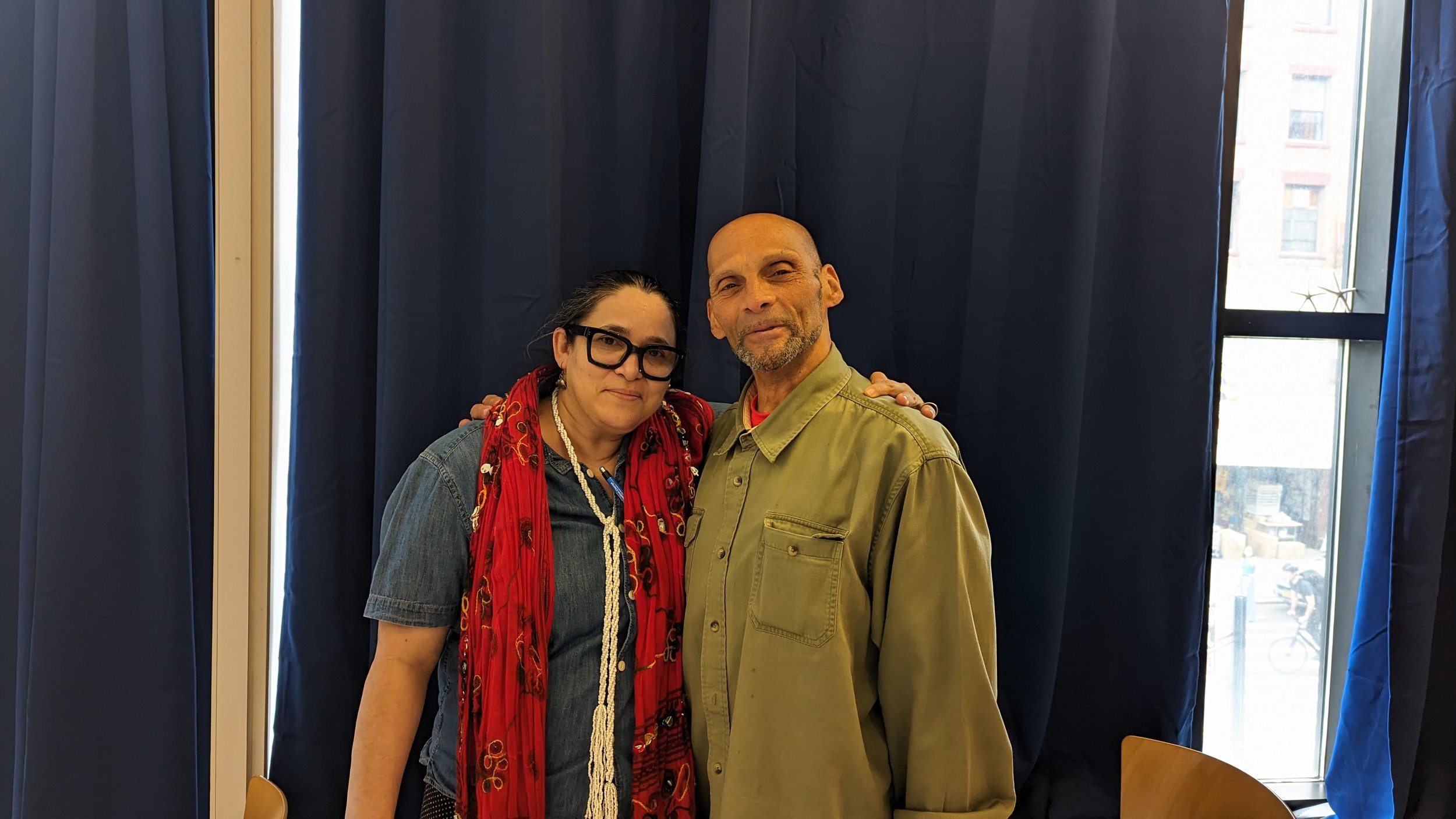
I’ve done a bunch of one-on-one sessions with Ana, talking about my traumas and what led me to take these steps to stop using. I’ve had to deal with the fact that I’ve lost friends to overdoses, one guy injected himself in the neck because all his other veins were all used up. He died right in front of me. It takes a while to process stuff like that.
What do you want to do when you’ve completely stopped using?
I want to travel. Right now I’m restricted, because of the methadone. I can’t go to a graffiti competition in Chicago, because I don't want to have to deal with the backlash from missing a few sessions of Methadone.
I want to go back to Puerto Rico, I have so many great memories of being there, in the countryside. Because I really love nature. I grew up around horses and roosters, and I loved it. I want more time to focus on those things.
You’ve mentioned being around nature, and animals. What are some of your other hobbies?
I love being outdoors most of all, and everything outdoors, like fishing, camping, hiking, horseback riding, all that stuff. I have an aunt down in Maryland that I’d visit because she was near all these different rivers so I’d swim all these places, anywhere! I’ve held big snapping turtles, and alligators, it’s exciting, man! I love nature.